Crohn's Disease in Older Adults: Understanding Postoperative Recurrence Risks and Biologic Prophylaxis Benefits
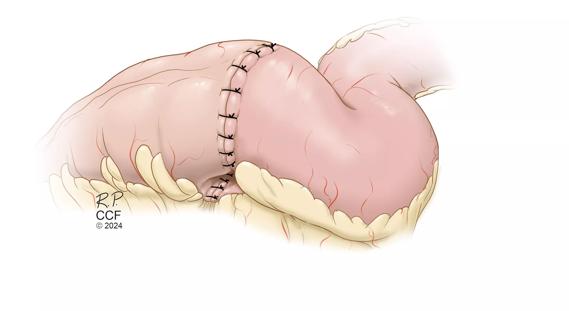
A recent nationwide study, in collaboration with Cleveland Clinic, sheds light on the increased risk of postoperative recurrence (POR) in older adults with Crohn's disease following ileocolic resection (ICR). The research underscores the significant impact of biologic prophylaxis in reducing recurrence risk, while also highlighting the disparity in its usage among older patients.
Why is Postoperative Recurrence a Concern in Crohn's Disease?
Postoperative recurrence after ileocolic resection is a common challenge in Crohn's disease management. This study aimed to investigate recurrence rates and risk factors, especially in older adults, where data has been limited. Understanding these risks is crucial for tailoring effective treatment strategies and improving patient outcomes.
Key Findings: How Age Impacts Crohn's Disease After Surgery
The study, presented at Digestive Disease Week, involved analyzing data from 1,095 Crohn's disease patients undergoing ileocolic resection between 2009 and 2020. The cohort was divided into younger (18-59 years) and older (≥60 years) groups. Here's what the research revealed:
- Increased Risk: Older patients with Crohn's face a significantly shorter time to composite postoperative recurrence at the 5-year follow-up, driven primarily by higher endoscopic POR rates.
- Biologic Prophylaxis Benefits: Initiation of biologic prophylaxis within 90 days of surgery significantly reduces the risk of both endoscopic and composite postoperative recurrence across all measured time intervals.
- Underutilization in Older Adults: Biologic prophylaxis was less frequently administered to older patients (23.6%) compared to their younger counterparts (31.3%).
The study also found that older patients often had longer disease duration, a stricturing phenotype, a history of tobacco use ,and prior ileocolic resection. Furthermore, while younger patients had more overall postoperative recurrence risk factors (70.5% vs 57.6%), the impact of recurrence appeared more pronounced in the older group.
Understanding Postoperative Recurrence: Endoscopic, Radiologic, and Surgical
In this study, postoperative recurrence was defined comprehensively, encompassing:
- Endoscopic Recurrence: Identified via Rutgeerts’ score ≥ i2b during ileoscopy.
- Radiologic Recurrence: Indicated by inflammation detected on imaging.
- Surgical Recurrence: Requiring a repeat ileocolic resection (redo ICR).
- Composite Recurrence: Defined as any combination of endoscopic, radiologic, or surgical recurrence.
Biologic Prophylaxis: A Powerful Tool Often Underused
The research highlights the effectiveness of biologic prophylaxis in preventing postoperative recurrence. However, its underutilization in older patients raises concerns. Historically, the concern for potential risks has led to a hesitancy for usage of biologic therapies in this age group. This study advocates for re-evaluating treatment strategies, pushing for individualized care, and moving beyond chronological age as the definitive factor in treatment consideration.
Clinical Implications: Individualized Treatment for Crohn's Patients
These findings emphasize the need to consider a patient's overall health and individual risk factors when making treatment decisions, rather than relying solely on age. Individualizing treatment for Crohn's disease in older adults means:
- Assessing individual recurrence risk: Evaluating factors beyond age.
- Considering biologic prophylaxis: Weighing the benefits against potential risks based on the patient's health status.
- Prioritizing patient-centered care: Tailoring treatment to meet the specific needs of each individual.
Long-Term Outlook: Improving Outcomes for Older Adults with Crohn's Disease
By adopting a patient-centered approach and considering biologic prophylaxis for high-risk older patients, healthcare professionals can significantly reduce the likelihood of postoperative recurrence and improve long-term outcomes for individuals with Crohn's disease. This research reinforces the importance of proactive and personalized management strategies for this patient population.